When Western medicine failed, these patients designed their own successful cannabis regimens
Cannabis was officially sanctioned by the Massachusetts Department of Public Health as a legitimate medical treatment in 2012. But because it is still illegal federally, clinicians are rarely taught about cannabis in medical school and are often barred from prescribing it or even talking about it with patients.
This has left patients in a quandary. They can access cannabis legally, but they get little clinical guidance. As a result, people have created their own treatment plans.
Speaking with advocates and people in the cannabis community, we identified and reached out to three patients who once believed strongly in Western medicine but had to defy it when an illegal plant proved to be the better option. Through trial and error, they created health regimens for serious conditions including epilepsy, multiple sclerosis, and chronic pain.
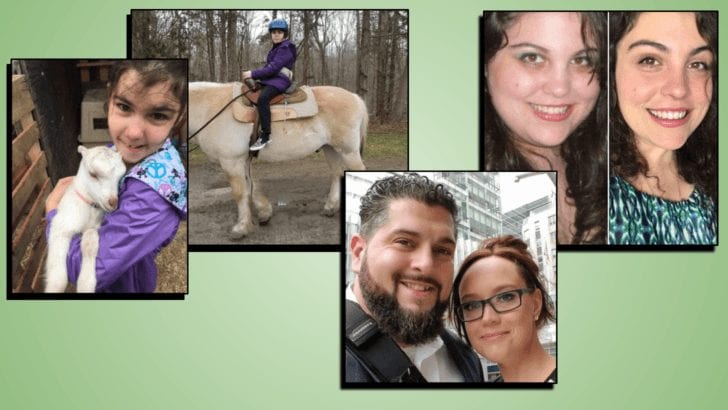
Liz Minda, a nurse who works in Western medicine every day, went completely herbalist with her daughter’s epilepsy. For her multiple sclerosis, Carolyn Kaufman took a holistic approach by mixing Western medicine and cannabis with an overall lifestyle change. Stephen Mandile, an Iraq war veteran, switched from opioids to medical cannabis for pain, depression, and PTSD, even though it meant risking his benefits at the Veterans Health Administration (VA).

JADYN MINDA (Epilepsy)
At 18 months old, Jadyn Minda experienced a febrile seizure. Over the next few years, she seemed fine—until she had another seizure at age four.
Then came an avalanche of seizures. Her mother, Liz Minda, a nurse at Kent Hospital in Warwick, Rhode Island, tried the traditional treatments, but nothing seemed to work. Every drug they put her on, even rescue drugs like Diastat, would cause more seizures. Jadyn was declining rapidly.
As a nurse, Minda was a believer in Western medicine, but she was uncomfortable putting Jadyn on drugs, particularly benzodiazepines. She knew their long-term use caused decreased brain function, liver damage, hormonal dysfunction, and an overall weakening of the immune system. She started to look at other options. She heard cannabis had potential, and was interested in trying it, but she couldn’t fathom the idea of Jadyn puffing on a joint. Plus, it was still illegal.
Then came Sanjay Gupta’s CNN documentary, Weed, in 2013. When she learned that cannabis could be taken as an oil, it became a realistic option. By then, Jadyn had tried and failed 10 pharmaceutical drugs and gone through six years of battling the disease. Minda and her husband knew they’d be “stepping out of their comfort zone to say the least” in trying cannabis.
It was a tough transition. “For me to walk in the opposite direction as allopathic medicine was very hard. But I would watch cannabis stop the seizure right before my eyes. There was no doubt in my mind, but it was very scary because I didn’t have the medical profession to support me.”
Weaning Jadyn off pharmaceuticals would require a protocol. Jadyn’s pharmacists and doctors couldn’t advise. She met a scientist out of California through an online forum of parents with epileptic children. He gave her a basic protocol to wean Jadyn off the drugs. Jadyn needed all the cannabinoids from the plant, including the psychoactive cannabinoid THC. Within three weeks of starting cannabis, Jadyn was off three pharmaceuticals.
Unlike pharmaceuticals, cannabis never sedated Jadyn to the point of respiratory arrest. With the benzodiazepines and the rescue drugs, Jadyn couldn’t function, but with cannabis she remained present.
“I could get her seizures under control and, although cannabis would sedate her, she could still eat, she could talk, she could follow verbal commands, she could still engage with her eyes and walk with assistance,” Minda says.
Jadyn has been two years off all pharmaceuticals. Now she relies solely on hemp oil, which she takes three times a day, and emergency THC oil to quell unexpected seizures. Jadyn’s daytime seizures are under control. She has been able to attend Coventry Public School and keep up with her class. Should she have a seizure, a drop of the THC oil placed between her lip and gum does the trick. Minda hopes that someday Jadyn will be able to take the THC while she is at school. Currently, it is illegal to use cannabis on a public school campus in Rhode Island.
They eventually found a cannabis-friendly doctor in John Gaitanis, MD, chief pediatric neurologist at Tufts Medical Center. Gaitanis has been willing to support Jadyn through her cannabis treatment, even though she is his only patient not taking pharmaceutical drugs. Having someone “in the system” is helpful for the exams, lab work, and moral support, but Minda says she and her husband are still on their own in terms of dosing, what levels of compounds like THC and CBD to give Jadyn, and how to administer it.
That’s no surprise; in a 2017 study published in the journal Drug and Alcohol Dependence, researchers found that fewer than 1 in 10 medical schools included medical cannabis in their curricula. Two-thirds of medical school deans reported that their graduates were not prepared to prescribe cannabis, and a quarter were not prepared to answer questions about it.
There are some signs of improvement. According to a 2018 study conducted by the Dana-Farber Cancer Institute and published in the Journal of Clinical Oncology, nearly half of US cancer doctors who responded to a survey say they’ve recently recommended medical cannabis to patients, although most say they don’t know enough about medicinal use because of the lack of research. They also stated that patients were usually the ones to bring it up.
Minda is now an activist helping other parents going through this.
“Jadyn will never get those valuable five years back,” she says. “I am angry, frustrated, disappointed, and broken-hearted for Jadyn, and all the others kids suffering. … The war on drugs is extremely misguided, at the very least.”
Jadyn Minda’s Regimen:
- Pure CBD hemp oil three times a day—15mg or 25mg of a CBD capsule.
- Before bedtime: an OG Kush indica raw flower in food.
- Pure THC oil as a rescue method for unexpected seizures.
- A CBD patch if necessary.

CAROLYN KAUFMAN (Multiple Sclerosis)
Carolyn Kaufman is the last person you would expect to reject cannabis as a medical treatment. Her first impression of it as a teenager was when her brother got sick and cannabis was the only thing that worked for him. Her parents were supportive. She even wrote her college thesis on the medicinal properties of cannabis.
Still, the influence of Western medicine and the stigma against cannabis were so strong that when she was diagnosed with Multiple Sclerosis at 20 years old, even someone who believed cannabis was a legitimate medicine used it as a last resort.
MS is an autoimmune disease that damages the protective covering around nerves along the brain and spinal cord. Resulting nerve damage disrupts communication between the central nervous system and the body. For Kaufman there was pain, migraines, spasms throughout her body, and hypersensitivity on her skin.
“I had damage that created muscle spasms in my rib cage,” she recalls. “I remember they left me in a fetal position on my bathroom floor for three to 19 hours at a time, a few times a week.”
Complicating the situation, she weighed 360 pounds, so Kaufman’s doctor didn’t want to put her on steroids. Instead, he prescribed anti-seizure pills, anti-anxiety pills, muscle relaxants, and pain pills. Muscle relaxants, which were supposed to relieve the spasms, didn’t hit the central nervous system; they went straight to the muscle. They didn’t help with pain but rather just sedated her. She was not able to function at her job or daily activities.
Showing little improvement after nine months, Kaufman grew frustrated.
“I’d had enough,” she says. “I was with my brother at a friend’s house and was desperate for relief. I smoked, and in 20 minutes the pain dissipated.”
The stoner stigma still made it difficult for her to accept cannabis as a treatment for herself. “I didn’t think it was part of my personality to smoke pot,” she says. But it was hard to deny the value of cannabis as it helped her come off all of her symptom management medications. She soon adopted a wellness plan that included cannabis, and her symptoms became manageable.
Complicated diseases with wide-ranging symptoms that vary per patient, like MS or fibromyalgia, require trial and error, a process that is usually easier when a certified healthcare practitioner is involved. Cannabis patients are on their own, and Kaufman had to learn how to use cannabis strategically. Over time, she adopted practices of integrative medicine. While she still takes a MS modifying drug, she also has radically changed her lifestyle with exercise, a strict “energetic” diet, meditation, and cannabis.
“This is my medicine. I feel so much gratitude,” Kaufman says. “I’d been feeling so shameful of something that is only helping me.”
Kaufman currently works as a mindset coach at her own business, Without the Weight, and contributes to the cause as a cannabis advocate. If her clients use cannabis, she says they often need to know how to make these health practices work in their lives.
“When it come to MS, you’re not supposed to get better once you’ve gotten sick,” she says. “I did. You’re not supposed to lose 140 pounds while smoking pot everyday. I did.”
Carolyn Kaufman’s Regimen:
- For diet, she eats energetically with fast-digesting carbohydrates for breakfast for energy; a lunch with moderate fat, protein, and slow-digesting carbs to sustain her; and a dinner with lean protein and vegetables to sleep well.
- For exercise, Kaufman goes to the gym regularly and, if needed, smokes beforehand to avoid muscle spasms.
- She prefers a sativa-dominant strain for daytime and an indica-dominant strain at night.
- Daily MS modifying drug.

STEPHEN MANDILE (Spinal Cord Injury, PTSD, Depression)
In 2005, public cannabis advocate, Stephen Mandile, was lead vehicle in a convoy in Iraq. His Army National Guard unit was bringing a prisoner to Abu Ghraib. Because of the threat of IED bombs, it was policy that convoys not stop for anything. Most Iraqis knew to stay out of the way, but not that day, and his truck tore out the back of a civilian car that crossed their path. The next morning, Mandile woke up and couldn’t move from his waist down. He had ruptured six discs in his spine.
Mandile took his honorable discharge and came home. Doctors told him that he could expect to be in a wheelchair by 50.
From 2010 to 2015, Mandile was prescribed 57 different medications, which that included opioids, muscle relaxants, and antidepressants. “Doctors said mourn who you were, just move on with who you are now. I didn’t know who I was now. And trying to figure that out on drugs like fentanyl was tough. Psychiatrists would ask how did I feel and I was just, like, ‘I don’t.’”
After a suicide attempt in 2013, Mandile’s wife insisted that he look into cannabis. She was working at MCI-Framingham, a women’s prison, and saw women having withdrawal symptoms from opioid abuse that looked like what he was experiencing when his fentanyl patch wore off. At first, he was offended. Mandile had always associated weed with slackers. But the other foreseeable option—potentially overdosing or worse—helped him make the decision. “My choice was medical heroin or medical cannabis—tens of thousands of deaths, or no deaths.”
In 2013, Mandile wanted to start consuming, but there were no dispensaries open. That changed in June 2015, and after five months of excruciating withdrawal, he was off all synthetic medications.
In December 2015, Mandile had an epiphany. He decided to try shoveling his driveway for the first time since the accident in Iraq. He thought he would just do a small path. An hour later, he had shoveled the entire driveway. With cannabis, his pain was manageable. He says he was also able to focus. He decided at that moment to become a cannabis activist.
This wasn’t easy for someone in his position. If veterans test positive for cannabis, the VA can cut their benefits. The VA also tests to make sure people are taking the opioids they are given and not selling them.
“I was so fed up,” Mandile says. “I survived Iraq, and I survived these pills. Talking to my doctor is the last thing that I should be afraid of.”
It is not illegal for VA doctors to recommend cannabis to patients in legal states like Massachusetts. Nevertheless, internal VA policy has been reluctant to allow this until cannabis is federally legal. Luckily, Mandile’s VA doctor was open to it, and helped him withdraw from the medications.
In addition to his advocacy, Mandile is part of a research and development group at Evergreen Farms, a grow facility in Bellingham, Massachusetts. The program helps disabled veterans get the help they need at reduced cost. Mandile would like to see the state open a location for alternative healing, where cannabis could be grown, packaged, and given to veterans, along with opportunities for other therapeutic activities.
Stephen Mandile’s Regimen:
- Morning meditation.
- Take a high- CBD (cannabidiol) sativa strain in the morning—Harlequin.
- Gradually increase THC (tetrahydrocannabinol) throughout the day—Goji OG.
- Mindfulness training.
- Exercise.
- At night take 200 mg of THC for sleep—Granddaddy Purple (high indica).
- Administration: inhalant and edibles.
- Medication for gout.
—///—
If federal prohibition ends in the United States—and this seems likely—research on cannabis will grow as restrictions fall away. Medical schools will integrate it into their curricula. Patients will not be so alone in creating their treatment plans.
But what will be lost? Some patients like how proactive they have to be with their cannabis treatments because it makes them feel empowered. And the fact that it’s practically impossible to overdose on cannabis makes self-medicating relatively less scary. As Mandile puts it, “With pot, you can take it based on how you feel, not like pharmaceuticals where you have to take it every four hours or whatever, no matter what else is going on with your body. The worse that will happen to me if I have too much cannabis is I take a nap.”
Patients also like how treatment with cannabis involves the whole plant, all the natural chemical compounds working together in a synergistic phenomenon known as the entourage effect. Liz Minda was told to use whole plant cannabis oil when she helped Jadyn withdraw from the pharmaceuticals and she believes that was crucial. In contrast, the pharmaceutical industry typically extracts compounds separately to create a chemically prepared product such as Marinol, a synthetic THC. The federal government is taking the middle ground. In May, a House committee approved cannabis law reform legislation that would encourage the VA to conduct research on whole plant cannabis as well as extracts.
The future of cannabis treatment may follow two parallel tracks: herbalism or Western medicine. But more likely these tracks will merge. As with Carolyn Kaufman’s integrative regimen, cannabis will likely become part of a personalized treatment plan that pulls from a range of therapies.